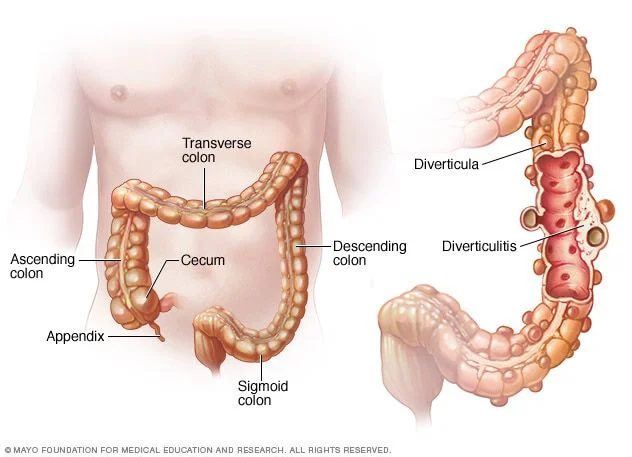
Diverticular disease, often referred to as Diverticulosis, is the presence of sacs or pockets in the inner lining of the colon.
Diverticula can develop when there is pressure on a weak area of the bowel wall; and therefore diverticular disease is common alongside constipation. Other risk factors include age; smoking, low fibre intake and use of some drugs including steroids. It is important to note that evidence also suggest some people are genetically predisposed to diverticular disease. Whilst you cannot cure Diverticular disease you can manage your symptoms and reduce the likelihood of a flare up.
Diverticula themselves do not cause symptoms and you might have had them for many years without knowing. As you can see from the picture it is easy for waste products to get trapped in these pockets which can cause inflammation or infection and associated symptoms including vomiting, abdominal pain, fever and change in bowel habits and blood in stools.
Photo credit: Mayo Foundation for Medical Education and Research
If you are experiencing a flare up and are symptomatic with fever, significant abdominal pain and/or blood in stools I would advise you contact your GP who might advise you start a course of antibiotics at home or be admitted to hospital for intravenous antibiotics.
Cognitive Behavioural Therapy
In a word, no!
It is common for individuals diagnosed with Diverticular disease to find the dietary advice confusing. Many report receiving little to no dietary information upon diagnosis, leaving them uncertain about whether to incorporate fibre into their diet to effectively manage their gut and bowel symptoms. This confusion can lead to challenges in understanding how to best support their overall health and well-being.
The dietary guidelines for individuals with diverticular disease closely resemble those for the general population. If you do not experience any symptoms, there is no need to eliminate specific foods from your diet. However, it is important to pay close attention to the amount and type of fibre, as well as your fluid intake, to ensure regular, soft bowel movements and to prevent symptoms and flare-ups.
Based on current recommendations, the suggested daily fiber intake ranges from 18-30g, derived from a diverse range of sources including whole grains like oats, fruits, vegetables, and pulses. During an acute flare-up of diverticular disease, it is advisable to reduce your total fiber intake and switch to a different type of fiber to effectively manage loose stools and abdominal pain. This modification, alongside careful monitoring of fluid intake, can help alleviate symptoms and support overall gut health.
Let’s break this down a little further…
There are two different types of fibre that you can include in your diet: insoluble and soluble fibre. Insoluble fibre provides bulk to your stools and can be found in wholegrain products like seeded bread, nuts, seeds, and the skins and stalks of fruits and vegetables, such as the woody stalk of kale leaves and the skin of apples. On the other hand, soluble fibre is found in the flesh of fruits and vegetables, as well as in oats, linseeds, and pulses like chickpeas. Soluble fibre acts like a sponge, soaking up water to keep the stool soft, allowing for easier passage through your bowel.
Nutrition and lifestyle tips to support a regular bowel movement include:
- Opt for porridge oats in the morning or as the warmer weather arrives try some overnight oats to boost your soluble fibre intake
- Add 1-2 tsp ground or whole linseeds to your cereal, yogurt, soups and stews. Ensure you have an extra 150mls water at the same time
- Smoothies are a great way to boost your fruit and vegetable intake. A great smoothie choice is banana, strawberries, spinach, greek yogurt, milk and spoonful of peanut butter.
- Include more pulses in your diet e.g. add red lentils to shepherds pie, chickpeas to your salads or curries
- It is also important to drink plenty of fluids when increasing your fibre intake.
- Exercise or physical activity also helps to prevent constipation by increasing muscle contractions in your bowel.

Will I have to just eat a beige diet when in a flare up?
If you are in a flare up you are likely suffering with pain, nausea and diarrhoea. However you do not need to avoid all fibre and limit yourself to beige foods. By making small changes to your diet you can help manage your symptoms but also feel reassured you are getting a good supply of nutrients
If you suffer from regular bouts of diverticulitis you might benefit from reducing your intake of insoluble fibre temporarily as foods containing pips, seeds, and skins are common culprits for getting trapped in the diverticula pockets. Insoluble fibre can also irritate the gut and contribute to pain therefore simple switches include replacing wholemeal bread with white bread, choosing more refined cereals such as cornflakes instead of branflakes, and removing woody stalks from vegetables.
You can still include soluble fibre in the diet and good options include using smooth nut butter instead of chunky nut butter or hummous instead of whole chickpeas. Homemade soups and sauces are a great way to include vegetables in the diet and by blitzing them you mechanically break down the fibres but still retain the nutrients.
If you are confused over how to manage your diverticular disease I would love to advise and support you to find a way to manage your symptoms and continue to enjoy a wide variety of foods. The gut game changer package would be a perfect fit for you to allow time to discuss your symptoms and devise a tailored plan to help you feel better and in control of your symptoms
Get in touch here or email me at hello@victoriadeprez.co.uk