Histamine is a chemical released by the immune system and is involved in many body functions. Everybody needs histamine to survive but when things go wrong and histamine levels are too high the whole body can be affected.
People commonly think of histamines in relation to anti-histamines, the medication used to treat allergy symptoms caused by having too much histamine in their bodies. However Histamine has many roles other than helping your immune system respond to allergy triggers; including acting as a neurotransmitter for the brain, dilating blood vessels and lowering blood pressure; and stimulating gastric acid secretion in the stomach. Histamine is an important chemical mediator but as we know you can have too much of a good thing… Could (undiagnosed) high levels of histamine be contributing to the unexplained increase in your heart rate, dizziness, diarrhoea, itching, constant runny nose, or persistent headaches? Read on to learn what histamine intolerance is, how it can be diagnosed, and what you can do to improve your symptoms.
What is Histamine Intolerance?
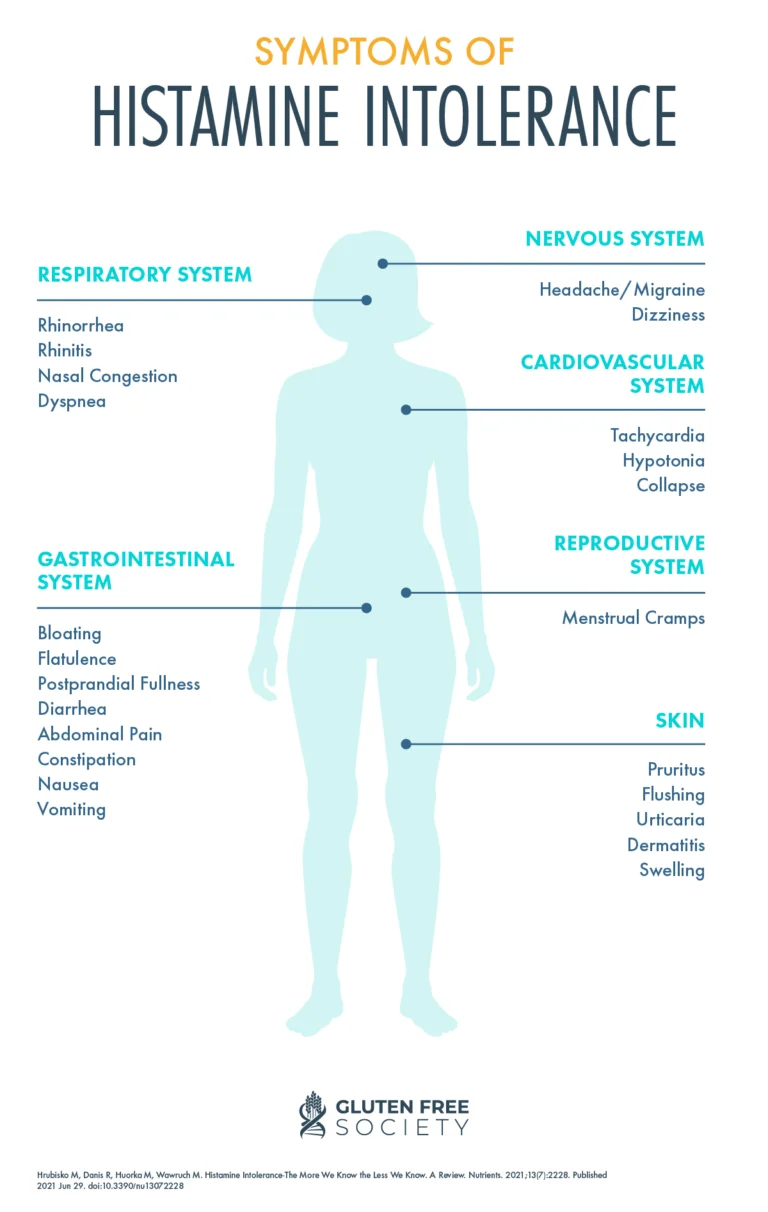
Histamine intolerance (HIT) is when there is an imbalance between the amount of histamine consumed in the diet and the body’s capacity to metabolise and get rid of it. Histamine levels may build up, causing a wide range of symptoms throughout the whole body including:
- Skin: hives, flushing, itching, swelling, eczema
- Respiratory: rhinitis (constant runny nose), nasal congestion, sinusitis, wheeze, shortness of breath, chronic cough
- Gut: acid reflux, nausea, constipation, diarrhoea, bloating, wind
- Vascular: dizziness, fainting, drop in blood pressure, migraine, oedema, heart palpitations
- Neurological: headaches, migraines, anxiety, brain fog, insomnia, vertigo
Many people with histamine intolerance experience various non-specific symptoms, which can make it difficult to diagnose and manage the condition effectively. It is important to consult with your GP to first rule out a primary IgE allergy before exploring further about histamine intolerance.
The body contains four histamine receptors, and the symptoms experienced can vary significantly depending on which histamine receptors histamine binds to. When histamine binds to H1 receptors (located in the brain, airways, and skin), typical “allergic symptoms” such as itching, narrowed airways resulting in shortness of breath, and increased heart rate may be noticed. On the other hand, if histamine binds more to H2 receptors in the stomach, individuals may experience gut issues including diarrhea, cramping, and bloating.
Symptoms can appear suddenly within 30 minutes or have a delayed reaction, depending on how full your histamine bucket is (more on that shortly). Moreover, you may feel fine for some time and then experience symptoms intermittently or continuously for no apparent reason. Many clients have reported being prescribed multiple medications for their symptoms that did not provide much relief, such as nasal sprays for nasal congestion or medication for abdominal cramps. How can these medications work if they are not addressing the underlying problem?
The wide range of symptoms and their timing further explains why it can take a long time and be a painful journey for a person to get diagnosed.
What causes histamine intolerance?
It is thought that there are two main reasons why people may experience Histamine Intolerance.
An overproduction of histamine in the body due to conditions such as Mast Cell Activation Syndrome (MCAS) and gut dysbiosis
Impaired histamine breakdown, which is proposed to be due to an impairment or deficiency in the enzyme Diamine Oxidase (DAO). Medications including ibuprofen, genetics, hormonal changes e.g. oestrogen and gastrointestinal diseases such as inflammatory bowel disease have all been shown to affect DAO enzyme levels.
Who is more susceptible?
Women are more likely than men to suffer with histamine intolerance than men and unfortunately this is due to their hormones which can play havoc with histamine levels. Women who I see in clinic commonly report changes to their sensitivity to histamine around their menstrual cycle and this is well documented, as oestrogen appears to increase the amount of histamine produced by mast cells and also stops the Diamine Oxidase (DAO) working as well. So as our levels of oestrogen fluctuate across our lifetime so too does our tolerance to histamine.

Women in their 40s who are perimenopausal experience fluctuating levels of 0estrogen. Perimenopause comes with a range of symptoms including hot flashes, mood swings, anxiety, joint pain, and heart palpitations, and these symptoms overlap with those of histamine intolerance, making life especially challenging for women with undiagnosed histamine intolerance during perimenopause.
Furthermore, some women who start hormone replacement therapy (HRT) and have undiagnosed histamine intolerance may suddenly develop new unexplained symptoms that resemble histamine intolerance, such as new allergies or intolerances, or an exacerbation of existing symptoms. This can make the already difficult menopausal experience even more challenging.
If this resonates with you, it’s important to consider the possibility of histamine intolerance. If you start HRT and notice that your symptoms worsen or develop new unexplained symptoms, histamine intolerance should be a consideration. If you experience worsened brain fog, more frequent headaches, unexplained increase in cramping, or changes in bowel habits, or if consuming cheese and wine makes you feel worse than before, it might indicate histamine intolerance as the underlying issue.
How is Histamine Intolerance diagnosed?
Due to the wide range of symptoms and overlap of symptoms with multiple other conditions there are no specific direct tests that can be used to determine histamine intolerance. Therefore the diagnosis of histamine intolerance typically requires the presence of two or more symptoms and improvement with a low histamine diet and/or antihistamines, and the exclusion of food allergies.
The gold standard way to diagnose histamine intolerance is to try and eliminate histamine as much as possible from the diet for a period of approximately 2-4 weeks. A strict low histamine diet is not a long term diet as it can increase your risk of nutritional deficiencies and will significantly reduce your invitations to your friends for dinner! The goal is to remove these high histamine foods from your diet and then reintroduce them gradually to see how often and/or how much you can tolerate. It is not just the type of food that is important but how the food is prepared, how old the food is. For example fresh chicken has a low histamine content but reheated chicken one or two days later will have a much higher histamine content.
It is best to embark on a low histamine diet with the support of an experienced Dietitian, particularly if there are other foods are being avoided to ensure the diet remains well balanced.
Foods high in histamine include:
- Aged foods including cheese, blue cheese
- Fermented foods such as sauerkraut, soy sauce, Kefir, blue cheese
- Drinks including alcohol, coffee, hot chocolate
- Vinegar
- Cured meats and fish
- Pork
- Vegetables including avocados, tomatoes
- Fruits including bananas, strawberries and citrus fruits , grapes
- Chocolate (milk and dark)

There is no universal list of high fodmap foods as many factors affect the histamine content of a food including the storage, freshness etc. Working with a dietitian who has experience with histamine intolerance can help you identify what your individual triggers are and create a meal plan that is low in histamine.
Is a low histamine diet all you need?
A low histamine diet can provide substantial relief for people but it does not address the root cause of the problem i.e. potential lack of histamine clearance or other factors that contribute to higher histamine levels and topping up your “histamine bucket”!
The histamine bucket can help to explain your own level of tolerance to histamine. Think of your body as an empty bucket and food, environmental factors such as hayfever, medications or stress can fill up the bucket. The more your bucket is full the more symptoms you might experience; and this helps explain why symptoms of histamine intolerance don’t always appear immediately but build up over time.
When your “bucket” overflows, that’s when you experience a reaction and that is why it is so difficult to identify your specific triggers and how foods/drinks/environment factors can affect you differently from one day to another.

What can you do?
- Track your menstrual cycle to monitor your hormone levels and determine if you notice a link between increased symptoms before your period. Consider if your symptoms have worsened since starting HRT as this could suggest undiagnosed HIT
- Create your stress busting strategy! Cortisol, a known “stress hormone” is known to increase histamine release.
- Consider low histamine diet with the support of a dietitian
- Cook food from fresh and store leftovers in the freezer, not the fridge
- Increase your intake of vitamin C and B6 rich foods as evidence suggests these 2 nutrients are important for histamine detoxification. Vitamin C rich foods include berries, kiwi and peppers and Vitamin B6 – fresh meat, potatoes, lentils and pulses
- Limit alcohol intake as alcohol contains histamine and also reduces DAO action so you might find you tolerate alcohol really poorly.
- Consider use of Diamine Oxidase Enzyme supplements. You can purchase capsules containing the enzyme diamine oxidase which can be used alongside a low histamine diet to allow more freedom with food and drink.
- Manage your medicine cupboard. Some medications interfere with your body’s ability to break down histamine or affect DAO activity e.g. NSAIDS such as Ibuprofen. You might wish to discuss trialling anti histamines with your GP, however some anti-histamines can exacerbate the symptoms as they interfere with histamine degradation. SPEAK with your GP before changing any medication.
How can I help?
If you feel overwhelmed with what to do next or are unsure if this is the right diet for you then get in touch. Working together we can discuss your symptoms and whether a low histamine diet is the right diet for you. Additionally i can equip you with a list of foods that are low-histamine and together co-create a personalized low-histamine diet plan for you with guidance on meal ideas, snacks and I can answer any questions and address concerns that you may have, either related to histamine intolerance or something else.